This case report presents the aesthetic and functional rehabilitation of a patient with increased overjet, a varied shade range (A1–A3), and a history of severe bruxism. The patient sought improvements in dental alignment and smile brightness. Clinical evaluation revealed anterior misalignment, inconsistent coloration, and occlusal wear consistent with chronic parafunction. A minimally invasive, no-prep approach using 80µm thick UltraThineer 5Y zirconia veneers addressed aesthetic concerns while preserving natural enamel. Functional elements, such as occlusal scheme adjustment and parafunctional protection, were integrated into the treatment. This case highlights the importance of comprehensive diagnostics and interdisciplinary planning in managing aesthetic cases with functional complexities.
Case Study
UltraThineer: From Average to Extraordinary
Developed by UltraThineer, In collaboration with Dr. Tai Ha, DDS, Newport Beach Dental Studio


Introduction
Restoring dental aesthetics in patients with underlying functional disorders, such as bruxism, presents a complex challenge that requires balancing cosmetic outcomes with long-term durability and biological preservation. Patients with parafunctional habits often exhibit signs of occlusal trauma, including enamel wear, incisal chipping, and altered bite dynamics, all of which must be carefully evaluated during treatment planning. Moreover, individuals presenting with increased overjet and tooth misalignment may also experience compromised aesthetics and function, further complicating restorative decisions. Traditional veneer techniques often involve enamel reduction, which can pose additional risks in cases involving already weakened dentition or occlusal instability. In response to these limitations, ultra-thin, no-prep veneer systems have emerged as a viable alternative for suitable patients, allowing for aesthetic enhancement with little to no compromise of tooth structure. These systems not only support conservative treatment philosophies but also provide a practical solution for patients desiring improvements in tooth shade, shape, and alignment without the need for invasive procedures.
This case report presents the interdisciplinary rehabilitation of a patient with a history of bruxism, overjet, varied tooth shade (A1–A3), and aesthetic dissatisfaction related to anterior disharmony and discoloration. Given the patient’s desire for a minimally invasive approach and improved smile aesthetics, 80µm thick UltraThineer 5Y zirconia veneers were sought out through the patient as the restorative modality. The treatment plan was carefully designed to integrate aesthetic enhancement with functional correction, including occlusal evaluation and post-treatment protection strategies to mitigate future parafunctional damage. This case underscores the clinical value of no-prep veneer systems in managing complex aesthetic presentations and highlights the importance of a comprehensive diagnostic process, material selection, and interdisciplinary collaboration in achieving predictable, long-lasting outcomes in high-risk functional cases.
Case Presentation
After contacting UltraThineer directly, the 36 year-old patient was referred to Dr. Tai Ha at Newport Beach Dental Studio in Newport Beach, California, for evaluation and management of her aesthetic concerns. The patient was firmly committed to improving her smile through a no-prep approach, which ultimately led her to discover UltraThineer as a no prep solution.
Chief Complaint: Aesthetic dissatisfaction related to anterior disharmony and discoloration.
Clinical Findings: Signs of bruxism were observed, evidenced by wear on the molars and anterior teeth. The patient was referred for a sleep study.
Diagnosis: Generalized attrition of anterior and posterior dentition associated with bruxism, increased overjet, anterior misalignment, and shade inconsistency (A1–A3), resulting in functional and aesthetic disharmony.
Treatment Plan
A comprehensive case history was obtained, followed by pre-operative photography, radiographic imaging, intraoral scanning, and a detailed clinical examination. After a thorough discussion of the patient’s aesthetic goals, the digital records were submitted to UltraThineer for case design and initiation of the 3D printing process. The patient expressed that she did not want a generic “perfect smile,” but preferred to preserve the unique characteristics of her original smile. Pt also expressed she did not want orthodontics. The treatment plan includes the upper 10 and lower 6 units (canine to canine). The patient’s current tooth shade ranges from A1 to A3, with BL3 selected as the final shade to achieve a brighter, more uniform aesthetic. From a functional and aesthetic standpoint, minor alignment corrections were made to the maxillary anterior segment. The lateral incisors exhibit slight labial prominence; therefore, we will bring the central incisors and canines slightly forward to create a more harmonious arch form and improved incisal symmetry, all within UltraThineer design parameters.

Fig 1

Fig 2
Fig 3

Fig 4
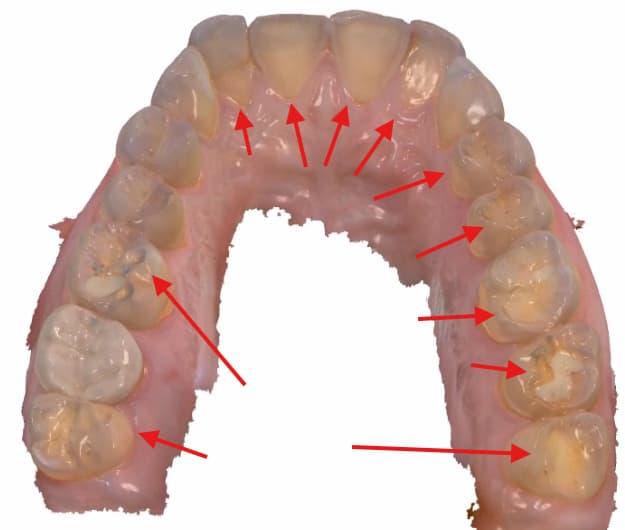
Fig 5
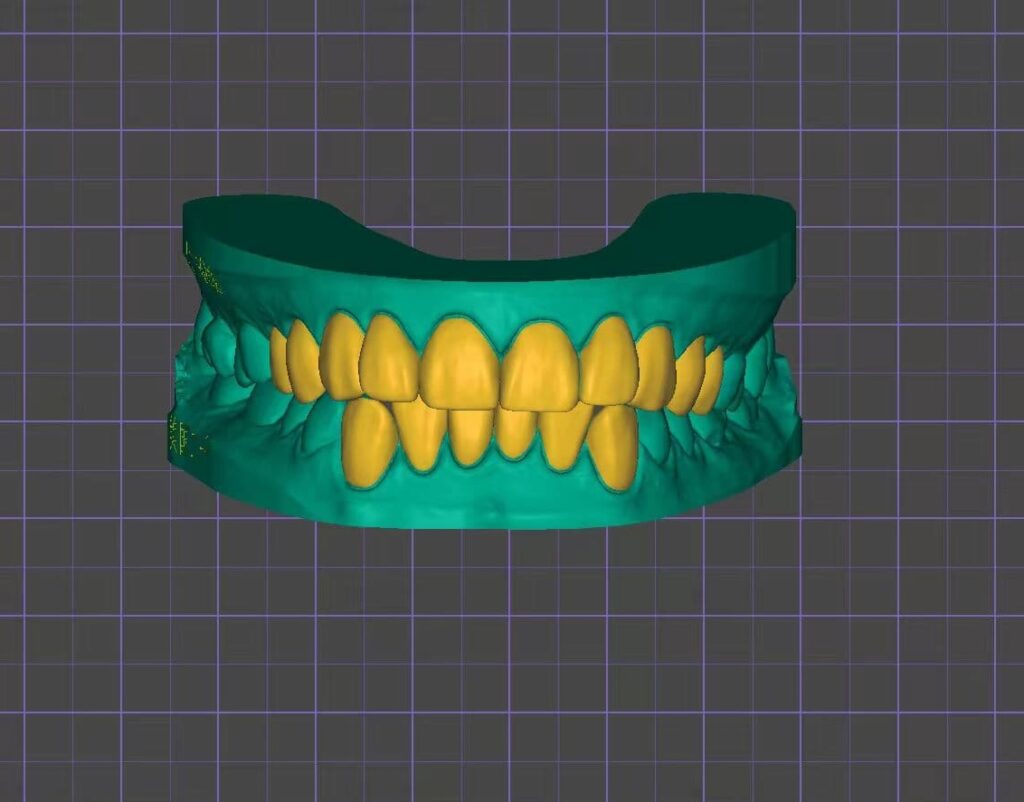
Fig 6
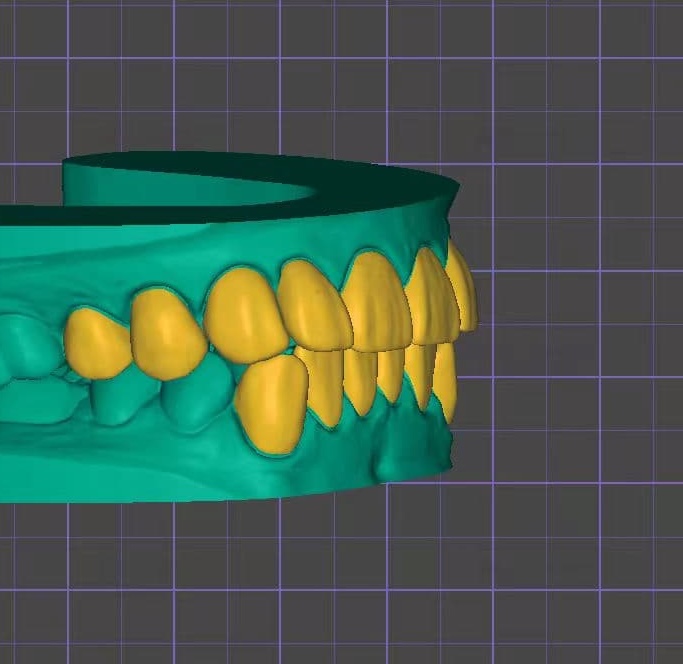
Fig 7
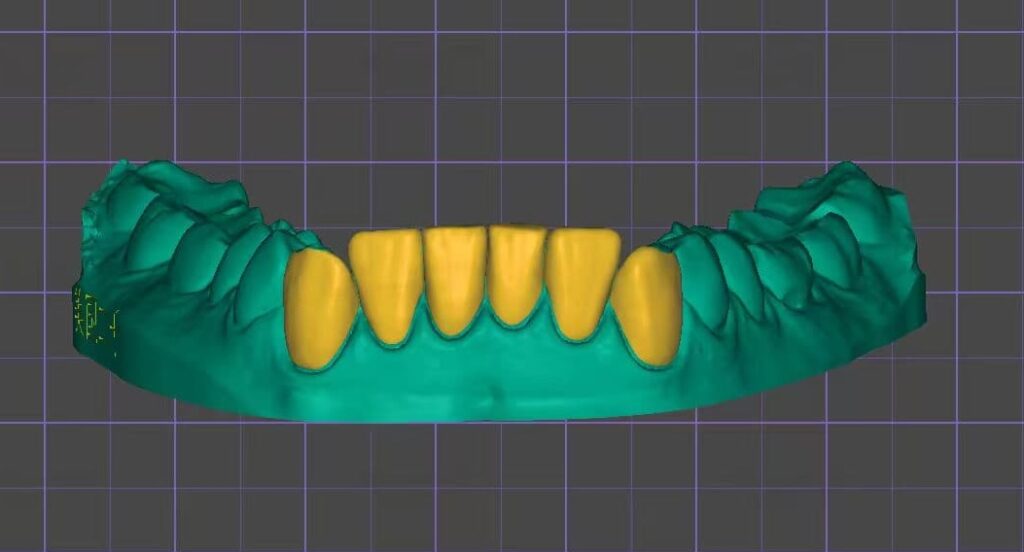
Fig 8
Treatment Procedure
The treatment began with a test fit of the veneers using a selection of colored cements. The veneers were then cleaned in an ultrasonic bath for 3 minutes and air dried. Next, 9.5% hydrofluoric acid was applied precisely for 60 seconds, including the margins, followed by another 3-minute ultrasonic cleaning. Two layers of porcelain primer (silane) were brushed onto the veneers, allowed to sit for 5 minutes, then air dried for 30 seconds. A thin layer of porcelain bonding resin was applied without light curing. The veneers were preloaded with permanent cement and protected under an orange shield after being warmed in the composite warmer. On the tooth surfaces, a plaque indicator was applied followed by fluoride-free pumicing and micro etching with 32% phosphoric acid. The teeth were then etched with 32% phosphoric acid for 30 seconds, rinsed thoroughly for 30 seconds, and 1 to 2 thin layers of All-Bond Universal adhesive were applied, air thinned, and light cured for a minimum of 10 seconds at 800 mW/cm2. The veneers were seated and tack-cured in place to stabilize positioning. Excess uncured cement was then carefully removed prior to final curing as cured cement is highly difficult to remove, especially interproximally. Once excess cement was removed, the veneers were light cured for 20 seconds. A 12-blade scalpel, interproximal saws, and scalers were used to remove and residual cement. Glycerin was then placed over the margins to prevent oxygen inhibition, and a final 20 second cure was done. After rinsing the glycerin, contacts and occlusion were checked, and final radiographs were taken. To prevent damage to the veneer margins, use of a handpiece around the facial margins was strictly avoided. Instead, residual cement was carefully removed using hand scalers and a #12 blade for optimal precision and margin integrity. The total delivery time for 16 veneers including seating, cement cleanup, radiographic verification, and occlusal adjustment was approximately 4 hours.
Outcome and Follow-Up

Fig 9

Fig 10

Fig 11

Fig 12

Fig 13
Discussion
This case illustrates the clinical challenges and opportunities in managing a patient with significant functional risk factors specifically, bruxism while addressing demanding aesthetic goals. Bruxism-related tooth wear not only compromises tooth morphology but can also contribute to occlusal instability, increased overjet, and loss of incisal guidance. These factors require careful planning to ensure long-term restorative success.
A key consideration in this case was the patient’s insistence on a no-prep approach. Conventional porcelain veneer therapy often requires significant enamel reduction, which can weaken remaining tooth structure and compromise bonding potential, particularly in bruxers where occlusal forces are excessive. By selecting UltraThineer zirconia veneers, we achieved a balance between aesthetic improvement and maximal preservation of enamel for optimal adhesion and longevity.
From an aesthetic standpoint, the treatment addressed both tooth shade and alignment discrepancies. Digital smile design allowed us to simulate subtle alignment corrections while preserving the patient’s natural smile character, a critical component in meeting her personal expectations. Functional refinements to the occlusal scheme were integrated into the design process to enhance long-term stability and reduce the risk of veneer chipping or debonding under parafunctional loads.
Post-restorative protection is paramount in such cases. Although veneers improve form and function, they do not eliminate the destructive potential of bruxism. The patient was referred for a sleep study to evaluate potential sleep-related breathing disorders that may exacerbate parafunctional activity. Additionally, an occlusal guard was recommended for nightly wear to protect the ceramics and preserve treatment longevity. This case reinforces the importance of interdisciplinary collaboration, combining restorative dentistry, occlusion management, and sleep medicine to produce predictable outcomes in high-risk patients.
Conclusion
This case demonstrates that minimally invasive, no-prep UltraThineer zirconia veneers can successfully address both aesthetic and functional demands in a patient with bruxism, increased overjet, and shade inconsistencies. The use of UltraThineer zirconia veneers allowed for enamel preservation, strong adhesive bonding, and precise control over smile design without sacrificing structural integrity.
Successful outcomes in such cases require:
- Comprehensive diagnosis of both aesthetic and functional conditions.
- Digital planning to align treatment outcomes with patient expectations.
- Functional considerations such as occlusal optimization and parafunctional protection.
- Interdisciplinary care when underlying sleep or occlusal disorders are suspected.
By combining conservative veneer therapy with functional risk management, clinicians can achieve lasting aesthetic results while safeguarding the health of the dentition in patients with complex restorative needs.
References
- Manfredini, D., Winocur, E., Guarda-Nardini, L., Paesani, D., & Lobbezoo, F. (2013). Epidemiology of bruxism in adults: A systematic review of the literature. Journal of Orofacial Pain, 27(2), 99-110.
- Fahl, N. (2007). A polychromatic composite layering approach for solving a complex anterior esthetic dilemma. Journal of Esthetic and Restorative Dentistry, 19(2), 63-76. https://doi.org/10.1111/j.1708-8240.2007.00082.x
- Lobbezoo, F., Ahlberg, J., Glaros, A. G., Kato, T., Koyano, K., Lavigne, G. J., Winocur, E., & Svensson, P. (2013). Bruxism defined and graded: An international consensus. Journal of Oral Rehabilitation, 40(1), 2-4. https://doi.org/10.1111/joor.12011
