Case Study
Zero Prep, Maximum Impact with UltraThineer
Developed by UltraThineer, In collaboration with Dr. Jessica Raber, DMD, Flawless Dental
Abstract
This case report details a minimally invasive approach to correcting minor aesthetic deficiencies without removing any tooth structure. The primary concern was chipping and incisal edge wear of the maxillary anterior teeth, accompanied by discoloration. Additionally, the patient sought to enhance the overall shade, starting from 2L 1.5 on the Vita 3D Shade guide. A no-prep technique utilizing 80μm-thick UltraThineer 5Y zirconia veneers was chosen to achieve the desired aesthetic improvements while fully preserving the natural enamel.
Introduction
Managing minor aesthetic imperfections such as incisal edge wear, chipping, and discoloration poses a challenge when aiming to maintain tooth structure. Traditional veneer preparations often require enamel reduction, which can compromise the longevity of the tooth and increase treatment complexity. No-prep or minimal-prep veneers made from ultra-thin zirconia offer a conservative alternative that meets patient demands for improved smile aesthetics while preserving natural enamel. This approach aligns with trends favoring minimally invasive dentistry and reversible treatments. The following case demonstrates the application of 80μm UltraThineer veneers to effectively restore function and appearance in a patient presenting with anterior tooth wear and discoloration, achieving aesthetic goals without compromising dental tissue.
When patients present with minor aesthetic concerns such as chipping, wear, or discoloration, the clinical decision often hinges on balancing effective results with tissue preservation. Advances in ultra-thin zirconia veneers now allow clinicians to offer minimally invasive, fully reversible treatments that respect natural tooth structure. This case explores the application of no-prep UltraThineer veneers as a viable solution to enhance smile aesthetics without compromising enamel integrity.
Case Presentation
Following an initial introduction to the UltraThineer team at the American Academy of Cosmetic Dentistry (AACD) April 2025 meeting, professional interest in the system remained high. Dr. Raber awaited a suitable case to explore the no-prep protocol offered by UltraThineer. Once an appropriate case was identified, the UltraThineer team was contacted to initiate the digital design process and establish patient expectations. A 47-year-old female patient presented to Flawless Dental in Newton Centre, MA, seeking evaluation and management of aesthetic concerns. Both the patient and Dr. Raber were aligned in their preference for a minimally invasive solution. The no-prep, 100% reversible nature of UltraThineer restorations offered an ideal treatment modality that met the patient’s goals.
Chief Complaint: Chipping and incisal edge wear of the maxillary anterior teeth, along with discoloration.
Clinical Findings: Clinical examination revealed incisal chipping on #8, an uneven incisal edge on #9, and discoloration of #11. A ceramic bridge was present from #4-6, along with a ceramic implant crown on #12.
Diagnosis: Moderate wear with intrinsic discoloration #5-11.
Treatment Plan
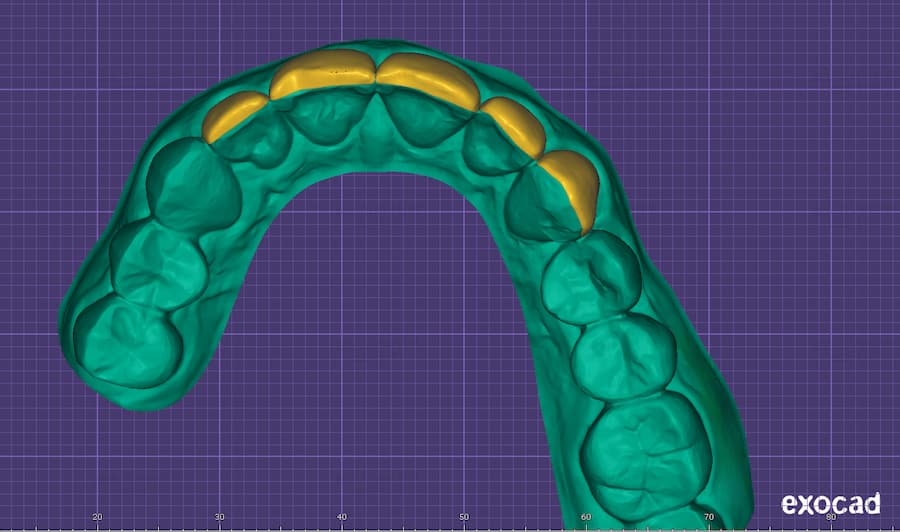
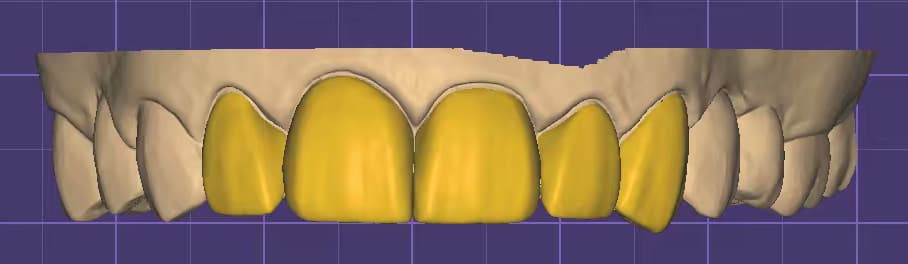
A comprehensive case history was obtained, followed by pre-operative photography, radiographic imaging, intraoral scanning, and a detailed clinical examination. After a thorough discussion of the patient’s aesthetic goals, the digital records were submitted to UltraThineer for case design and initiation of the 3D printing process. The treatment plan involved placing five upper veneers, extending from lateral incisor to canine; however, due to an existing bridge on the left side, the veneers were limited accordingly. The patient’s current tooth shade is 2L 1.5 (VITA 3D-Master Shade Guide) with A1 selected as the desired final shade to achieve a brighter and more uniform aesthetic outcome.
Treatment Procedure
The treatment protocol initiated with a trial placement of the veneers to assess marginal fit, adaptation, and esthetic integration prior to final cementation. A translucent shade try-in paste was applied to teeth #7 and #8, while shade A1 was applied to teeth #9 through #11 (Fig 8 and 9).


This allowed for a comparison of the shades to determine the best match and overall fit. The veneers were then cleaned in an ultrasonic bath for 3 minutes and air dried. Next, 9.5% hydrofluoric acid was applied precisely for 60 seconds, including the margins, washed with water into a neutralizing powder solution, then followed by another 3-minute ultrasonic cleaning. Two layers of porcelain primer (silane) were brushed onto the veneers, allowed to sit for 5 minutes, then air dried for 30 seconds. A thin layer of porcelain bonding resin was applied without light curing. The veneers were preloaded with permanent cement and protected under an orange shield after being warmed in the composite warmer. The teeth were then etched with 32% phosphoric acid for 30 seconds, rinsed thoroughly for 30 seconds, and 1 to 2 thin layers of All-Bond Universal adhesive were applied, air dried, and light cured for a minimum of 10 seconds at 800 mW/cm2. The veneers were seated and tack-cured in place for 1 second to stabilize positioning. Excess uncured cement was then carefully removed prior to final curing as cured cement is highly difficult to remove, especially interproximally. Each veneer was light-cured for 20 seconds. Ivoclar Liquid Strip (glycerin gel) was then applied and light-cured to eliminate the oxygen-inhibited layer. Following curing, the glycerin was thoroughly rinsed off. Contacts and occlusion were carefully evaluated and adjusted as needed, and final radiographs were taken to confirm proper seating and fit. The total delivery time for 5 veneers including seating, cement cleanup, radiographic verification, and occlusal adjustment was approximately 2 hours.
Outcome and Follow-Up
Discussion
This case demonstrates the successful application of a no-prep, ultra-thin zirconia veneer protocol to address minor anterior aesthetic concerns while preserving natural tooth structure. Traditional porcelain veneer techniques often involve varying degrees of enamel reduction, which may compromise tooth integrity and introduce long-term risks such as sensitivity or structural weakening. In contrast, the use of 80μm-thick UltraThineer zirconia veneers allowed for full enamel preservation while achieving an aesthetic and functional result.
The clinical challenges in this case included incisal edge chipping, wear, and intrinsic discoloration which are typically managed with ceramic restorations that may require aggressive tooth preparation. However, technological advancements in materials science have made it possible to fabricate ultra-thin restorations with sufficient strength, translucency, and marginal adaptation, even at minimal thicknesses. The 5Y zirconia used in UltraThineer veneers offers enhanced translucency while maintaining superior flexural strength, making it suitable for anterior esthetic cases without the need for enamel reduction.
Patient selection and expectation management were critical to the success of this case. The patient’s preference for a conservative approach aligned well with the no-prep protocol. A comprehensive diagnostic workup including clinical examination, shade selection, intraoral scanning, and digital smile design ensured that both esthetic and functional goals were met. Shade comparison prior to final cementation allowed for customized esthetic optimization, ensuring patient satisfaction.
Conclusion
This case emphasizes the importance of collaboration between clinician and laboratory. From the initial digital submission to the 3D printing and final veneer fabrication, coordination with the UltraThineer team ensured accuracy and high-quality outcomes. The overall delivery time of approximately two hours for five veneers demonstrates the efficiency achievable with streamlined no-prep workflows.
In summary, this case supports the growing push towards minimally invasive cosmetic dentistry. UltraThineer veneers, when properly selected and bonded, can provide a durable, esthetically pleasing, and reversible solution for patients with minor anterior aesthetic concerns. This approach respects the principles of conservative dentistry while meeting modern demands for enhanced smile design.
References
1. McLaren, E. A., & Whiteman, Y. Y. (2010). Ceramics: rationale for material selection. Compendium of Continuing Education in Dentistry, 31(9), 666–668.
2. Gracis, S., Thompson, V. P., Ferencz, J. L., Silva, N. R. F. A., & Bonfante, E. A. (2015). A new classification system for all-ceramic and ceramic-like restorative materials. The International Journal of Prosthodontics, 28(3), 227–235.